What Is a Poor-Quality Embryo?
Poor quality embryos, or embryos with a “C” grade, are often discarded by clinics and never really given a chance. In this post we’ll look at what goes into defining an embryo as poor quality and what their potential is for live birth.
What is a poor-quality embryo?
During IVF, many embryos can be created and in order to prioritize them for transfer the embryologist examines how they look under the microscope to grade them. Embryos with the best grade, or quality, are transferred first and embryos with the lowest quality are transferred last (or in some cases not transferred at all and discarded).
When ranking embryos there’s usually 3 tiers: good, fair and poor.
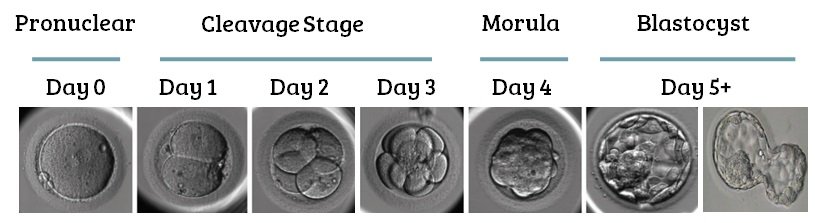
How grading is actually done depends on the stage of the embryo’s development. There are different criteria that the embryologist looks for in cleavage stage embryos (day 1-3) compared to blastocyst stage embryos (day 5+).
Poor quality cleavage stage embryo grading
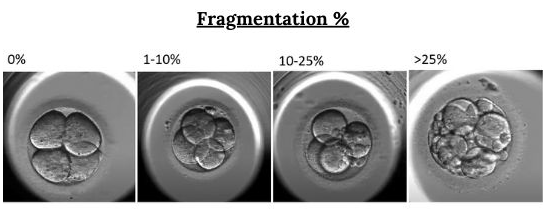
For cleavage stage embryos “fragmentation” is the critical thing to look out for. Fragmentation are tiny pieces of cells that break off of a cell and are scattered throughout the embryo. The more fragmentation there is, the worse the embryo’s quality. You can see increasing percentages of fragmentation below:
Besides fragmentation, the number of cells and symmetry of a cleavage stage embryo can also dictate its quality.
Poor quality blastocyst stage grading
For blastocysts, a poor-quality embryo is one that has a “C” quality score.
Blastocysts are graded using a system involving a number followed by two letters (ie. a 4BA):
The number indicates the blastocyst’s progression (4)
The first letter is the quality of the inner cell mass (B)
The second letter is the quality of the trophectoderm (A)
You can see a blastocyst below with its inner cell mass (ICM) and trophectoderm, along with the shell (zona) that’s used to evaluate the embryo’s progression/expansion:
The letters in the blastocyst’s grade can be A (good), B (fair) or C (poor). This has to do with the number of cells seen in the ICM and trophectoderm structures (more cells = better quality).
Generally, embryos with a C grade for either the ICM or trophectoderm are considered poor quality, and CC embryos are considered the lowest quality.
Clinics can have different ways in interpreting blastocyst scores. One clinic might consider a 4BC as fair quality, while another would consider it poor (i.e.. they might “round up”). A 4CA embryo might also be fair to some clinics (because A and C average out to a B).
It’s also up to the clinic to decide what to do with poor quality embryos. Many clinics have a threshold for what they consider acceptable to transfer or freeze and will discard embryos below that threshold, while other clinics will give every embryo a chance.
Let’s take a look at what the research says when it comes to the success rates or poor-quality embryos, and whether or not discarding them is justified.
Poor quality embryo success rate
Let's look at some representative studies for cleavage stage and blastocyst stage embryos.
Zhu et al. (2014) compared pregnancy outcomes after transferring 2 good or 2 poor quality day 3 embryos (good quality: 7-8 cells, <10% fragmentation; poor quality: ≤5 cells and/or 30–50% fragmentation):
Clinical pregnancy was decreased (50.26% vs 16.15%).
Live birth was decreased (39.60% vs 11.41%).
Miscarriage was increased (13.28% vs 19.77%).
No differences in stillbirths, ectopic pregnancies, neonatal complications, preterm birth, birth weights and other outcomes.
Bouillon et al. (2017) compared the transfer of a single good, fair or poor-quality embryo (good: AA, AB, BA; fair: BB; poor: CC, CB, CA, AC, BC):
Decrease in clinical pregnancy rates (55.6% vs 47.2% vs 43.6%).
Decrease in live birth rates (46.8% vs 39.0% vs 34.1%).
No statistical difference in miscarriages (13.7% vs 14.6% vs 18.7%).
No differences in ectopic pregnancies, preeclampsia, preterm birth, low birth weight, neonatal complications, congenital malformations and other outcomes
These are just a couple of studies, and others have found that poor quality embryos have about half the live birth rates compared to good quality embryos. Other studies have also found an increase in miscarriage rates, so that is something to consider when transferring poor quality embryos.
Why do clinics discard poor quality embryos?
Every clinic is different, and how they handle poor quality embryos can vary. Some clinics will gladly freeze or transfer every embryo produced in an IVF cycle, while others have strict requirements and will discard poor quality embryos (and often without informing the patient – however this will be indicated in the consent form).
Why this is isn’t clear.
One possible reason is because of the fierce competition experienced by IVF clinics. Patients will choose a clinic based on their success rates, which are made public. Centers that transfer poor quality embryos may have lower success rates because the embryos have lower success rates. Some clinics want to maximize their statistics by only transferring good/fair quality embryos.
Another possibility is that the clinic is simply unaware of the potential of these embryos. Transferring poor quality embryos may be more popular today than it was 20 years ago, and some clinics may just have a history of not transferring these embryos. As research comes out, it’s becoming clear that these embryos have a chance, and this is starting to change the perception of clinics.
The transfer of poor-quality embryos may have a reduced chance of live birth and an increased chance of miscarriage. For many patients’ poor-quality embryos may be a last resort for them, and patients deserve to be counseled on the risks and benefits of transferring these embryos.
Many patients have found success using poor quality embryos and I have a collection of IVF success stories on my website that demonstrates this.
For more information on this topic, check out Embryoman’s post on poor quality embryos and their success rates on his website Remembryo.
Author information: Embryoman is a former embryologist who now devotes his time to summarizing the latest IVF research in simple terms on his website Remembryo. He focuses on providing evidence-based information and has reported on many topics, including embryo quality, egg quality, sperm quality, and PGT-A. You can follow him on Facebook or Instagram.
Medical Disclaimer:
The information provided in this blog is intended for general informational purposes only and should not be considered as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider or qualified medical professional with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this blog.